Research Highlight | Groundbreaking Discoveries in Infectious Diseases

“If the drug works even half as well as what we’ve found to date, there would be nothing like it in the existing antimicrobials,” says Paul S. Hoffman, PhD, of UVA’s Division of Infectious Diseases and International Health and the Department of Microbiology, Immunology and Cancer Biology.
RESEARCH HIGHLIGHT/
Division of Infectious Diseases & International Health
Promising New Antibiotic Defies Conventional Wisdom on Treating Superbug
A new antibiotic to combat the dangerous C. difficile superbug, being developed by faculty members in the Department of Medicine’s Division of Infectious Diseases with colleagues from UVA’s Department of Chemistry and researchers from Virginia Tech’s Bioinformatics Institute, also appears effective against a wide array of other pathogens, including the Helicobacter pylori bacterium, a new study suggests. With antibiotic resistance a growing concern — and an alarming shortage of new antibiotics in development — the drug is notable because it works in a way that prevents microbes from becoming resistant to it.
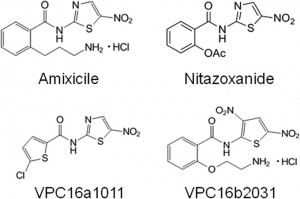
Infectious Diseases faculty member and lead investigator Paul Hoffman, PhD, says the new findings challenge conventional wisdom that the best way to develop new treatments for Clostridium difficile, a growing problem in healthcare settings nationwide, is to target that infection specifically and to use an antibiotic that concentrates in the gut. The drug, Amixicile, developed by his team does neither — yet early testing suggests it could be significantly more effective than existing options.
Sparing Good Gut Bacteria
Amixicile may prove particularly effective against C. difficile because, unlike other antibiotics, it spares beneficial probiotic and other beneficial bacteria. There is growing evidence to suggest that probiotic bacteria help prevent C. difficile reinfection and relapse, so antibiotics that concentrate in the gut and kill off the intestinal flora indiscriminately make it easier for C. difficile to regain a toehold. Mice infected with C. difficile that were treated with other antibiotics commonly relapsed and died, but there were no relapses in mice treated with Amixicile, the researchers report.
Unlike other C. difficile therapeutics, Amixicile concentrates in the bloodstream, rather than in the gut, and emerges only at infected sites. Thus, Amixicile may be useful in treatment of systemic anaerobic and parasitic infections as well as gastric infections caused by H. pylori. More broadly, because of its low toxicity and immunity to mutation-based drug resistance, it potentially could be used as a lifelong prophylactic to prevent flare-ups of chronic diseases such as Crohn’s disease and ulcerative colitis. It may even prove effective against anaerobes associated with periodontal disease.
“If the drug works even half as well as what we’ve found to date, there would be nothing like it in the existing antimicrobials,” said Hoffman, who has a joint appointment in the Division of Infectious Diseases and in the Department of Microbiology, Immunology and Cancer Biology.
Amixicile avoids the problem of mutation-based drug resistance by its unusual mechanism of action. Amixicile targets the function of the vitamin B1 cofactor of pyruvate, ferredoxin oxidoreductase, an enzyme uniquely found in anaerobic pathogens and not present in humans or in the probiotic beneficial gut bacteria.
The vitamin cofactor, a small molecule, is not susceptible to mutation, offering a remarkably reliable — and therefore very attractive — target. Because the target won’t change, the risk of bacteria becoming resistant to the antibiotic is lessened dramatically.
Next Steps
More preclinical work needs to be done before the researchers can gain FDA approval to begin testing Amixicile in people. They next intend to evaluate maximum tolerable doses in animals and examine whether the drug has any genetic or mutagenic effects. If all goes well, they will eventually proceed to human testing.
The researchers’ latest findings have been published online by Antimicrobial Agents and Chemotherapy, a journal of the American Society for Microbiology:
Hoffman PS, Bruce AM, Olekhnovich I, Warren CA, Burgess SL, Hontecillas R, Viladomiu M, Bassaganya-Riera J, Guerrant RL, Macdonald TL. Preclinical studies of amixicile, a systemic therapeutic developed for treatment of Clostridium difficile infections that also shows efficacy against Helicobacter pylori. Antimicrob Agents Chemother 2014 08;58(8):4703-4712. DOI: 10.1128/AAC.03112-14
From UVA Today, July 25, 2014, by Josh Barney
Creating Immunity to Deadly E. histolytica
There are two common approaches to protecting humans from infectious disease: targeting pathogens and parasites with medicines such as antibiotics, or dealing with the conditions that allow transmission. Exciting research from the Division of Infectious Diseases & International Health, published in Nature‘s open-access, online journal, Scientific Reports, demonstrates the effectiveness of a third strategy: adjusting the landscape of the human body to remove the mechanism that allows pathogens to cause disease.

Study co-authors (l-r) William Petri Jr., MD; Hans Verkerke; and lead author Chelsea Marie, PhD; (co-author Dan Theodorescu not pictured).
A team led by ID postdoctoral fellow Chelsea Marie, PhD, was able to silence genes within human cells to induce immunity to the parasite E. histolytica, which infects 50 million people and causes 40,000–110,000 deaths via severe diarrhea worldwide each year. “This amoeba is a cluster bomb — a voracious killer,” says Dr. Marie, noting the challenge the researchers faced in blocking the amoeba’s ability to kill human cells. “In the back of my mind I was thinking the parasite was going to decimate the host cells no matter what we did with their genetics.”