Medical Education
The Department of Medicine plays an essential role in the School of Medicine’s education and training programs at all levels, with thousands of DOM faculty hours devoted to teaching and mentoring medical students, residents and fellows. In addition, many faculty members serve in leadership roles and on a variety of teaching and curriculum committees in the School of Medicine. They contribute to UVA’s Continuing Medical Education programs as well, providing content and leadership for many CME-sponsored courses and conferences.
Over the last two years, the Department of Medicine’s vice chair of education, Gerald R. Donowitz, MD, together with administrative director of graduate and undergraduate medical education, Joy Hilton, led a department-wide effort to centralize and streamline administrative processes for educational programs; education coordinators from each of the ten divisions meet regularly with Hilton and her team to develop best practices and share expertise. They also provide mentoring and direction for those newly hired into administrative positions with responsibility for divisional educational programs.
Medicine Clerkships

Medical Students
The medicine clerkship is designed to provide medical students with a basic fund of knowledge about common clinical problems and disease states encountered in the practice of inpatient and outpatient internal medicine. They learn to apply that knowledge in a wide variety of settings, developing the analytical and clinical skills necessary for the practice of evidence-based, cost-effective medicine. They gain experience in the use of consultants, the coordination of ancillary healthcare services, and the critical assessment of medical information, among many other areas.
Internal Medicine Residencies
The Department’s Internal Medicine residency program consistently attracts outstanding candidates from across the country. It provides a balance of hands-on patient care and cutting-edge research opportunities, with faculty who highly value their roles as mentors and teachers. The program is resident-centered and unequivocally resident-run – as evidenced by innovations such as the night float system and the current service structures that were designed and implemented by residents. The aim of the program is to guide residents in developing their individual interests and strengths, while building up their knowledge base and core clinical skills. To this end, a variety of training tracks are offered:
- Categorical: The traditional track emphasizing training in general internal medicine, with a focus on subspecialty and hospital-based practice.
- Primary Care: Designed for individuals wanting a career in general internal medicine (in either academic or clinical practice). Primary care residents spend an increasing proportion of time over their three years in the ambulatory setting, designing elective experiences to meet their training needs and interests.
- Preliminary: A one-year program that allows individuals to gain a broad experience in internal medicine before continuing in other medical disciplines. Includes inpatient rotations on the General Medicine services, Medical Intensive Care Unit, Coronary Care Unit, Hematology-Oncology, and Digestive Health.
- ABIM (American Board of Internal Medicine) Research Pathway: For individuals with extensive research interests and academic subspecialty career goals, this pathway consists of two years of training in the categorical track followed by one or more years of clinical training in a subspecialty, and at least five years of research training. It is offered in the subspecialties of cardiovascular disease; endocrinology, diabetes & metabolism; infectious diseases; and nephrology.
Over the last five years, approximately 75% of residency graduates have gone on to subspecialty fellowships, while the remainder have pursued careers in general internal medicine. Of those, more than half are working as hospitalists; another 45% work in outpatient primary care settings.
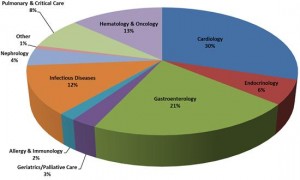
Of graduating residents who pursue subspecialty fellowships, the highest proportion (about 30%) are in cardiology, followed by gastroenterology (21%), hematology-oncology (13%), infectious diseases (12%), and pulmonary-critical care (8%), as shown in the pie chart.
Subspecialty Fellowships

Instructing fellows: Emaad Abdel-Rahman, PhD, MBBS
In the 2012-2013 academic year, 81 fellows were enrolled in 11 subspecialty programs and three sub-subspecialties. With the addition of a fellowship in heart failure during the last year, the department offers a total of 14 ACGME-accredited fellowship programs, in: allergy & immunology; cardiovascular disease; cardiovascular imaging; clinical cardiac electrophysiology; interventional cardiology; heart failure; endocrinology, diabetes & metabolism; gastroenterology and hepatology; geriatric medicine; hematology and oncology; hospice and palliative medicine; infectious diseases; nephrology; pulmonary disease and critical care medicine; and rheumatology.
In September 2012, two of the department’s fellowship programs – the Hospice and Palliative Care Medicine program, and the Transplant Hepatology program – received site visits from the ACGME. Both received reaccreditation through January 2017.